Meet Amy Harris from South Australia. Amy’s story is long as she’s been going through the symptoms of menopause since she was 28. She’s now 54.
“I began having problems in my 20s when my period changed. From lasting for about three days, and being long and light, they began arriving every day with cramping and pain. There were only a few days per month when I wasn’t bleeding.
In addition, I went on to have difficult pregnancies, lost my second child and my third child broke my pubic bone 14 weeks before he was due. As a result, I had to stay in hospital for the next 12 weeks but the baby was born six weeks early. Following the birth, I couldn’t walk for quite a while,” says Amy.
Amy has her tubes tied
Consequently, Amy was advised to have her tubes tied. Despite that, she continued to have problems.
While undergoing a laparoscopy, Amy was diagnosed with endometriosis. Then, when she asked to have her tubes untied so she could try for another baby, her doctor suggested she undergo a hysterectomy.
Surgically induced menopause
“So, at 28, I had my uterus and womb removed, but a year later I was still suffering from pain. They discovered that my right fallopian tube had fused to my bowel and my left tube and ovaries were covered in cysts. After that finding they removed the cysts, which put me into surgically induced menopause.” Since then, Amy has experienced many of the common symptoms of perimenopause such as hot flushes and mood swings. “As a matter of fact, the entire time I’ve been talking to you, I’ve been hot flushing,” she says.
Developing rheumatoid arthritis
The doctors tried me on a hormone implant but it didn’t work, so at 31 I went on HRT. However, it made me sick and gave me migraines,” says Amy. She also developed rheumatoid arthritis, which led to hip replacement surgery at just 42. At the time of writing, Amy had also just had lower spine surgery and her left shoulder needs to be replaced. “This is because my bones aged as I couldn’t take the HRT,” she says.
The final upshot
Amy’s story of menopause has been and continues to be, a long and arduous journey.
How does Amy cope?

“You adapt and get on with it. I’m a strong woman and I choose to take deep breaths and walk away. I hope my story helps others who – for whatever reason – may be suffering from the effects of menopause and are feeling alone.”
Hat tip to you for sharing your difficult journey, Amy.
A note on hysterectomy
A note on endometriosis
https://www.healthnavigator.org.nz/health-a-z/h/hysterectomy/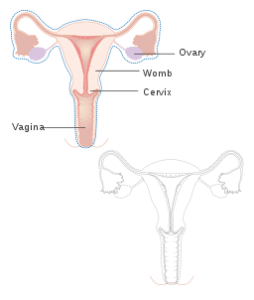
Generally, a hysterectomy is an operation that removes your uterus (womb). However, there are varying degrees of the procedure.
Subtotal: the main part of the uterus is removed but the cervix remains so you will still go through menopause naturally.
Total: a total hysterectomy removes the uterus and cervix but leaves the ovaries intact. As a result, you will still go through ‘natural’ menopause albeit it may occur earlier.
Extended: An extended (or full) hysterectomy removes the uterus and its surrounding tissue as well as the ovaries and fallopian tubes. In this case a woman will go straight into menopause.
This is known as surgically-induced menopause and, rather than a slow progression, you enter it abruptly. The data shows that many of the common menopause symptoms can be more severe when they occur as a result of medical intervention. (Another cause of ‘induced’ menopause can be chemotherapy.)
Source
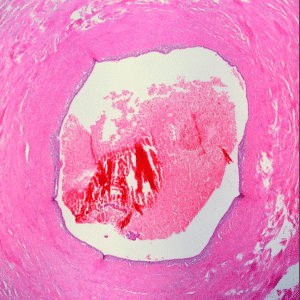
Endometriosis of the fallopian tube. Image Source
Endometriosis is a common inflammatory disease and it’s estimated to affect 176 million women and girls around the world.
According to nzendo.org.nz 120,000 females in New Zealand suffer from the condition. What’s more, Endometriosis Australia (EA) says there are currently 830,000 ‘Endo Warriors’ in Australia.
The symptoms of endometriosis can include period pain, pelvic pain, bowel problems, sub-fertility, infertility and fatigue. Occasionally, in some cases, none of the common signs occur. In fact, EA says it can take up to six years for women to be diagnosed.
Endo comes about when tissue similar to the lining of the uterus (endometrium), appears in places outside the uterus. This errant tissue can form nodules or plaques and is usually found in the pelvic region. It may also develop on the pelvic ligaments, ovaries and bowel. Source
At this time the cause of endometriosis is not fully understood, however the most compelling evidence points to genetics playing a large role. As well as this environmental and immunological factors are also being researched.
Endometriosis & menopause
According to the experts, endometriosis symptoms can improve after menopause as reproductive hormones decline. However, the body continues to produce small amounts of estrogen so for this reason symptoms may continue in some cases.
Endometriosis Australia lists 10 facts all women should be aware of:
- There is no cure for endometriosis.
- Teenagers are not too young to have it.
- Period pain is not normal.
- Hysterectomy is not a cure.
- Endo cannot be treated.
- It does not always cause infertility.
- Getting pregnant will not cure endometriosis.
- Surgical intervention is the only way of reaching a diagnosis.
- Pain levels don’t related to the extent of the disease.
- You cannot catch endometriosis; it is not an STI.