The Signs & Symptoms of Menopause
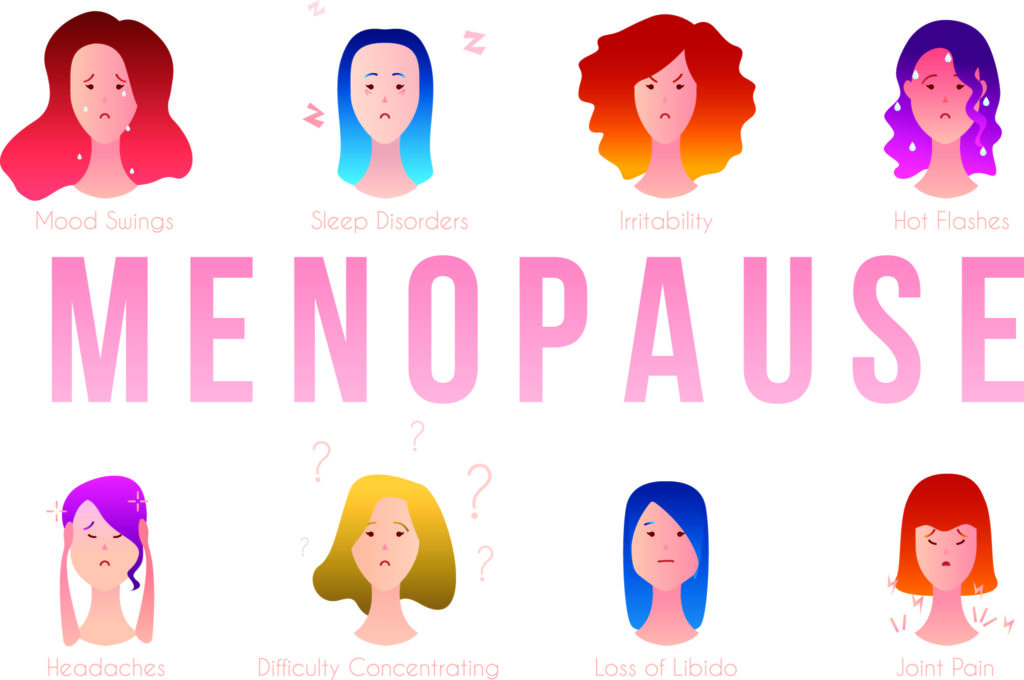
Table of Contents
What are the signs and symptoms of menopause?
You had ‘the period talk’ when you were hitting puberty right? But did anyone ever give you ‘the menopause talk’? If you’re like most of us, probably not. Never fear – we’ve done the intensive sleuthing and we’re about to cover off ‘the talk’ and jump right into the symptoms of menopause. Just think of us as your fairy-meno godmother!
First up, when we’re asking what the signs and symptoms of menopause are we’re really talking about perimenopause. These are the years preceding menopause itself and when most symptoms occur. In ‘doctor-speak’ it’s often called the ‘menopausal transition’.
The signs can be both physical and psychological and are due to hormonal imbalance. Menopause is not a ‘one size fits’ all process – it affects all women differently.
What’s happening as you enter perimenopause?
Your ovaries are older, your egg supply is dwindling and your most powerful sex hormones – most notably estrogen and progesterone – are declining. So even though you may still be getting a period you’re not necessarily ovulating. Progesterone drops markedly in our 30s and ovarian estrogen levels diminish in perimenopause. This usually begins in your 40s but rather than gradually fading out, estrogen goes through significant highs and lows a little like a rollercoaster.
These fluctuations can lead to estrogen dominance at times and hormone imbalance much of the time. The result? Symptoms like hot flushes, mood swings and tender breasts. Perimenopause is often compared to puberty but unlike the relative freedom of adolescence, you’re usually drowning in a sea of adult responsibility: career, kids, ageing parents, financial pressure, divorce, or perhaps your own or a partners health concerns.
With that said, many women sail through natural menopause with hardly a blip on their radar – lucky them! They may only notice their periods slightly changing and then ‘poof’ they’re gone. But for about 65-70 per cent of females, the 34 symptoms of menopause can be unpredictable and emotionally, mentally and physically fraught. Indeed, the signs can be intense for some especially if menopause has been brought on abruptly due to surgery, chemotherapy, or radiation.
These ladies may struggle with heavy or irregular periods, hot flushes, night sweats, sleeplessness, aches and pain, loss of libido, weight gain, thinning hair, irritability, low mood, concentration lapses, anxiety, dizziness, mood swings, fatigue, facial hair and anger. Phew!
Let’s shout about it
Perimenopause needs to be shouted about. You may have assumed your 40s would be a time to take stock before you’d need to think about menopause in your 50s. But peri can make it a decade that’s not as [hormonally] straightforward as you’ve imagined so it’s important to be savvy where your hormones are concerned.
The Menopause Numbers
Approximately 25 million women transition through menopause every year. By the year 2030, it’s estimated this will be 1.2 billion with 47 million new entrants to the menopausal fold annually.
It’s all good
All of this information shouldn’t send you running to a cave, nor should it cause younger woman to quiver with fear. In fact, it’s a good idea to share these pages with every woman you know. Menopause is a natural life stage – not an illness or disease. and the key to navigating it with ease is to look after your hormonal balance.
Here’s the truth: no one knows how the menopause transition will affect an individual woman. Every. Body. Is. Different. Some ladies are more sensitive to declining sex hormones than others. And knowledge is power. When you know what you’re dealing with during the menopause transition you can take steps to emerge victoriously and with a few safe tools and some lifestyle adjustments, you will.
Know the 34 Symptoms of Menopause
Now that we’ve got the ‘perimenopause talk’ out of the way let’s take a look at the common signs reported by peri- and post-menopausal women. The most well-documented are hot flushes (aka hot flashes) but don’t be fooled into thinking if you aren’t experiencing them you’re not in menopause – there are 34 recognised symptoms of menopause.
The Australasian Menopause Society tell us that 60 per cent of women will have mild symptoms for around four to eight years. Twenty per cent of women will have no symptoms at all while another 20 per cent will be severely affected, with symptoms continuing into their 60s or later.
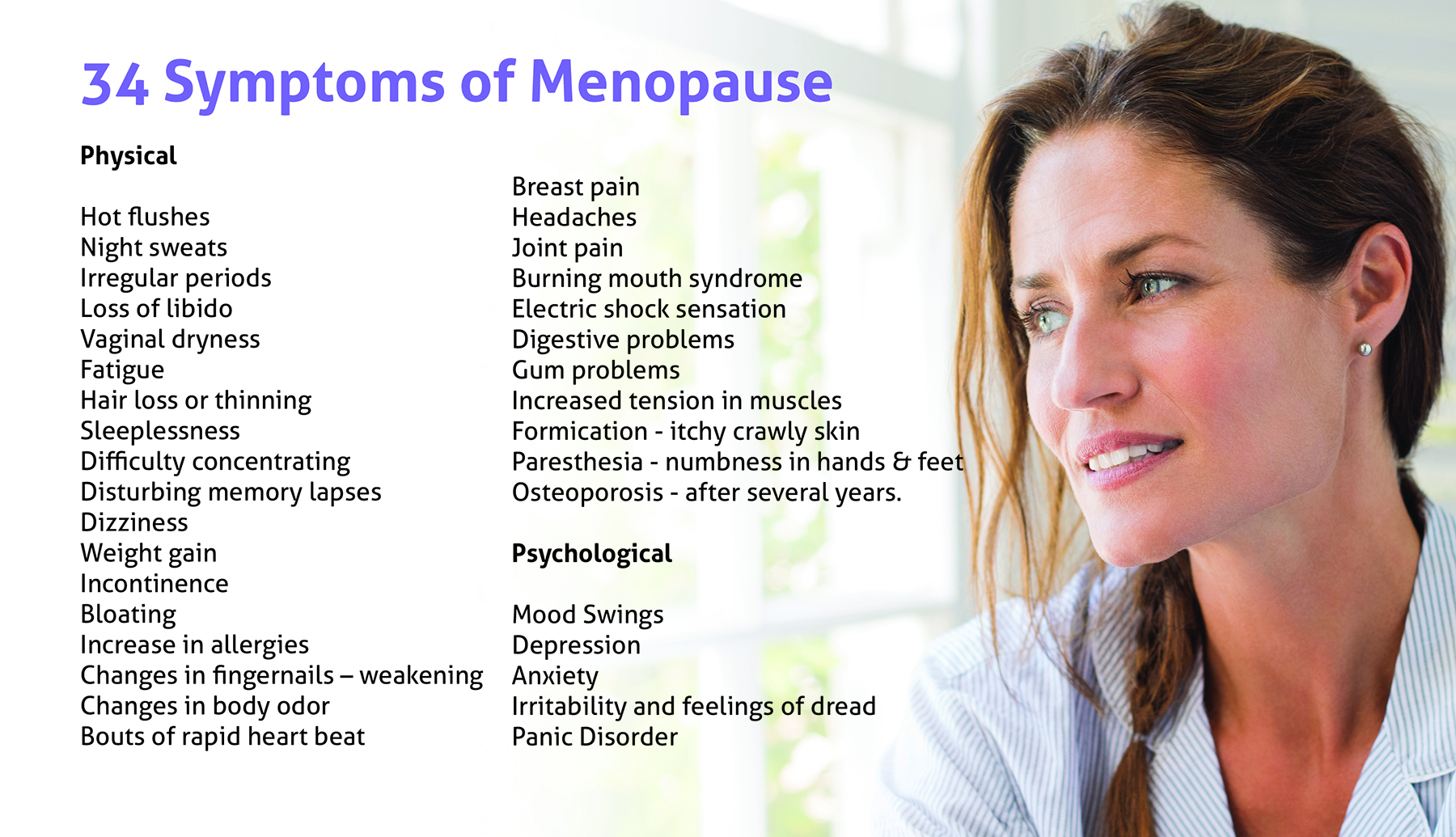
Physical Symptoms of Menopause
1. Allergies
As the hormones and the immune system are linked, allergies can present with more regularity during menopause.
2. Bloating
Perimenopausal women often experience an increase in bloating. It can feel similar to PMS, a hard, distended tummy and often (sorry) an increased incidence of burping or farting.
3. Body Odour Changes
This one’s often a surprise but decreasing estrogen levels can alter the pH level of the vagina. An overall change in natural scent is also linked to hormonal changes and sweating associated with body temperature changes during menopause.
4. Brain Fog
Difficulty concentrating, memory lapses (where have I put my keys?) and mental blocks are all part of what is – quite literally – a feeling as if your brain is foggy.
5. Breast Tenderness
Many of us have experienced the feeling of tender breasts and increased breast size during menstruation and/or pregnancy. These can also be common signs of perimenopause.
6. Burning Mouth Syndrome
A sensation of ‘burning’ on the tongue, the roof of the mouth or inside the lip area can be attributed to lower estrogen levels which lead to sensitivity and reduced production of saliva.
7. Digestive Issues
As we mentioned under bloating, signs of gas along with cramping, and sometimes nausea can be due – in part – to an underperforming gut.
8. Dizziness
A drop in estrogen may cause women to experience loss of balance, vertigo, a feeling of spinning and/or dizzy spells.
9. Electric Shock Sensations
It sounds unusual, but some women have said they feel an electric shock sensation under their skin. These often follow a hot flush.
10. Fatigue
Feelings of extreme exhaustion or a complete loss of energy are common.
11. Formication
Some menopausal women report feeling like they have bugs crawling on their arms and legs.
12. Hair Changes
A frustrating sign for women is thinning hair on their head and other parts of their bodies accompanied by an increase in facial hair.
13. Headaches
Hormonal headaches are a ‘thing’ and if you experienced them during your period you may be more likely to be affected by them during menopause. Even if you haven’t experienced them during menstruation they can be exacerbated in times of hormonal fluctuations.
14. Hot Flushes
This is probably the most infamous symptom of menopause recognisable by the heating up of the body/face and red flushing of the skin. Hot flushes can last for several years. They occur when the body’s natural thermostat goes awry due to hormonal fluctuations and in the brain’s bid to get everything back to normal this heat regulator causes a heatwave and sweating. Stress, spicy foods, caffeine, sugar and alcohol can be triggers.

15. Incontinence & UTI’s
Bladder leakage and control are one of those ‘shhh’ signs. Exacerbated by coughing or lifting heavy objects (stress incontinence) it can also show up as an uncontrollable compulsion to pee immediately (urge incontinence). More frequent urinary infections are not unusual as perimenopause progresses either.
16. Irregular Heartbeat
This gives new meaning to the phrase ‘be still my beating heart’, but it’s quite a common sign during perimenopause and can manifest as palpitations.
17. Irregular Periods
As we mentioned above, menstrual irregularity is often the first sign of perimenopause. It can show up as lighter, shorter periods or as very heavy bleeding.
18. Itchy Skin
Often not associated with the hormone imbalance of the menopause transition, itchy skin can be a side effect of fluctuating hormones. We frequently refer to estrogen as our ‘juice’ and as such it contributes to collagen production, a protein that keeps our skin plump and hydrated. When this is diminished skin becomes dry and itchy.
19. Joint Pain
Unfortunately, many women put joint and muscle discomfort down to exercise. Not surprisingly they don’t connect the dots that it’s a common sign of perimenopause. As estrogen plays a role in joint lubrication and is also an anti-inflammatory a reduction can cause stiffness and increased inflammation.
20. Loss of Libido
Not feeling ‘in the mood’ isn’t uncommon post-40. This can be distressing and cause issues in relationships. The paradox is that while many women experience a decrease in their libido some report a stronger sex drive.
21. Muscle Tension
A feeling of increased muscle tension may not be due to your workout but a result of hormonal fluctuation or increased stress, anxiety and/or levels of the stress hormone cortisol.
22. Night Sweats
Many females complain about this menopausal sign, which wakes them in the middle of the night contributing to fatigue. It’s attributable to the same physical mechanism that we’ve mentioned under hot flushes.
23. Oral Problems
Some women experience increased problems with bleeding gums and tooth loss during perimenopause. Another common symptom is a metallic taste in the mouth.
24. Osteoporosis
This becomes a serious risk at menopause. Osteoporosis (meaning porous bone) is a skeletal disease characterised by weakened bones and increased risk of bone fractures. The prevalence of osteoporosis is on the increase and affects more than half of females over 60. We lose bone mass two to four times faster after menopause – 10 per cent of it in the first five years of post-menopause. For more detailed symptom information click here.
25. Paresthesia
It’s an unusual word, isn’t it? It refers to ‘tingling extremities’ because it’s a sensation often felt in the hands, arms, feet, and legs. Women describe it as a feeling of numbness, a burning sensation or ‘pins and needles’. Estrogen has a role to play in the function of our central nervous system and a drop or variability can trigger paresthesia.
26. Sleeping Difficulties
Sleep disturbances, night sweats and insomnia often become an issue during menopause due to hormonal imbalance and hot flushes. Also, sweating from hot flushes during the night can make sleeping uncomfortable.
27. Vaginal Dryness and/or Atrophy
Because estrogen levels drop during menopause, a lessening of the vaginal ‘mucosa’ or our natural lubrication can cause vaginal dryness and in some cases dyspareunia (painful intercourse). As we’ve said before estrogen is our ‘juice’ and reduced levels lead to dryness in typically moist areas.
28. Weakened Fingernails
The hormonal fluctuations and declining estrogen associated with perimenopause, menopause and post-menopause can limit the body’s ability to produce keratin, resulting in brittle fingernails and toenails.
29. Weight Gain
One of the biggest bugbears of women at this age is weight gain. Especially ‘belly fat’. This is due to both hormonal and metabolic changes. The reasons can be complex and the key is lifestyle changes and education.
Psychological
30. Anxiety
Constant worry, concern and a sensation of dread in the pit of the stomach, the feelings of anxiety are out of all proportion to the normal sensitivities of everyday life.
31. Depression
Depression is serious and a big one for many women in menopause particularly if they have a history of clinical depression. The condition can go hand in hand with many of the mood changes of menopause. It’s important to realise this is menopause-related depression as opposed to clinical depression.
32. Irritability
Fluctuating sex hormones can cause a constantly shifting weight of mood changes. There are many comedic memes out there about this one, but all laughter aside it’s a common fact that perimenopausal women often become very irritable.
33. Mood Swings
Tears, joy, depression (see above), irritability (see above), rage – lowered estrogen can cause the pendulum to swing back and forth with mood variations in women. Studies have shown that about 23 per cent of women will experience mood swings.
34. Panic Disorder
Going one step further from irregular heartbeat and anxiety, panic attacks can also be a common symptom of menopause. They may manifest as shortness of breath, trembling or shaking, pounding heart rate and be accompanied by hot flushes and sweating.
What Can You Do About Your Menopause Symptoms Experience?
Diet & exercise
The food you eat is critical along with moving your body regularly in a way that works for you.

• Good Guts
In many ways, it all starts with the gut. It’s our digestive system that affects the production of hormones – melatonin (sleep) and serotonin (feel good) for example, are made here and gut issues often go hand in hand with hormonal imbalance.
• Eat Real Food
A Mediterranean-style diet abundant in fresh fruit and vegetables, olive oil, oily fish (salmon, sardines) and legumes (chickpeas, lentils, beans), along with phytoestrogens (soy foods like tofu and tempeh) are great choices for women in midlife. This way of eating predominantly plant-based with moderate amounts of dairy, seafood and red meat. (See 5 Ways Your Diet Should Change.)
• Say No To Junk
Refined foods like sugar-filled cakes and pastries and processed carbohydrates like white pasta and pastries can play havoc with your blood sugar and lead to insulin resistance and fat storage. Eating whole foods like those mentioned above helps to stabilise blood sugar. (See The Sugar Series.)
• Ditch The Liver Loaders
The liver is a very busy organ and one of its jobs is to metabolise hormones. When we drink alcohol and other liver loaders like caffeine, refined sugar and processed food, the liver will prioritise detoxing these. Having AFD (alcohol-free days) along with a ‘clean’ diet can free the liver up to concentrate on hormone work. The by-product of this is sunnier moods, more energy and better sleep. (See 5 Foods To Kick To The Curb.)
• Avoid Triggers
Hot flush triggers include alcohol, caffeine, refined sugar and stress.
• Move It
Exercising is one of the best things for our health – both cardio and strength training – to keep our skeleton and muscles strong, offset stress, promote good sleep and minimise symptoms. It’s important to exercise for at least 30 minutes per day and if you’re exercising for weight loss keep in mind that losing weight is 80 per cent about what you eat – exercise can’t burn off a bad diet and overdoing it will encourage fat storage. However, for overall health, weight and symptom management, moving your body is – along with a nutrient-dense diet – one of your best lifestyle tools. (See Why You Need To Exercise.)
Natural remedies
Ancient wisdom and modern know-how are both powerful forces and Mother Nature has a plethora of offerings for encouraging as non-symptomatic a menopause transition as possible.
• Acupuncture
Some ladies swear by acupuncture to ease hot flushes, night sweats and/or pain. This study backed up their positive claims.
• Appropriate Supplementation
Many women wish to be as non-medicalised as possible through the menopause transition and reach for natural supplementation like 40+ and 55+ to help ease their symptoms. Any supplements should be high quality, clinically tested with proven results and free of cheap fillers.

• Breath Work
Deep, abdominal breathing can reduce feelings of anxiety. One simple technique is to breathe in slowly for four counts, hold for seven, and breathe out for eight counts. Do this for a few rounds until you notice your anxiety subsiding.
• Cognitive Behavioural Therapy
CBT is often recognised as an effective treatment for women going through menopause to help improve hot flushes, sleep and mood swings. It’s a form of talking therapy that helps you understand your thoughts and how you feel.
• Ditch Smoking
Smoking is linked with going into menopause at an earlier age and a shortened life span. ‘Nuff said.
• Dress in layers and natural fibres
A hot flush can come on suddenly and cause intense discomfort. By dressing in layers you can peel off subtly to cool down. Wearing natural, breathable fibres such as cotton, silk, wool, cashmere and hemp will also help give cooling air access to your skin.
• Keep a cooling spritz on hand
Meet your new BFF – it could just be a spray bottle from the $2 store filled with water. Keep one in your car, your handbag and your fridge to bring instant relief during a hot flush.
• Meditation
Several studies show the efficacy of meditation for helping treat perimenopausal and post-menopausal symptoms.
• Mindfulness
Like meditation, mindfulness is a wonderful adjunct to easing menopausal symptoms.
• Pelvic floor exercises
Correctly performed pelvic floor exercises are helpful for women experiencing urinary incontinence. It’s also beneficial for post-menopausal women to increase their orgasm and sexual function.
• Use a cooling pad and/cooling towels.
Some ladies rave about the advantages of using a cooling pad on their beds and pillows to help alleviate the discomfort of night sweats. Similarly, portable cooling towels offer relief when used around the neck or the face and limbs.
• Yoga
Both women themselves and research studies have shown yoga to be beneficial for minimising hot flushes and psychological symptoms. Yoga is low impact but requires strength and resistance so is also good for building bone density and strength.
• Pilates
Like yoga, Pilates is beneficial for both mind, body and bone density at menopause. A small study of 110 post-menopausal Spanish females showed a 12-week programme had beneficial effects on sleep quality, anxiety, depression and fatigue.
• Don’t suffer in silence
This study found that family support and resilience contributed to fewer menopausal symptoms.

When to see a doctor
We always recommend making an appointment with your GP if you’re experiencing symptoms or if your period has ended over 12-months before and bleeding occurs again.
With that said, we know a lot of women go to see their GP and put the suggestion of menopause to them. Many are told they’re too young, others are prescribed antidepressants (some of which help with levels of estrogen) and others are told to grin and bear it. Still, others are subjected to a barrage of tests that all come back normal. As they should. Menopause is a normal part of life, it’s not a disease or an illness.
It’s also something that women feel they need support with but are uncomfortable talking about. The statistics are astonishing. A UK survey conducted on behalf of the British Menopause Society in 2016 found that only half of ladies consult a healthcare professional even though their symptoms have affected their quality of life.
To be very clear, we haven’t been to medical school and we’re not doctors but we have been told by those who have that general practitioner training doesn’t include a lot of lectures on menopause. Certainly, this article in the New England Journal of Medicine shows that medical training in the United States doesn’t prioritise it.
Fortunately, some doctors take a special interest in the subject, particularly if they’re a woman who’s been there. And specialist gynaecologists and endocrinologists should be helpful also. It pays to ask around for recommendations.
You Don’t Have To Go It Alone
There’s a need for more awareness and education. Menopause is the gateway to a new phase in life – a time when we can look forward to being free from periods, childbirth and (in all likelihood) the next third of our lives. Many women reinvent themselves or reach their full potential in the spirit of a super-strong sense of self. But it’s also a time when our health needs to take priority as we become more vulnerable to cardiovascular disease, osteoporosis and dementia.
Menopause matters. Heck, it’s being added to the school curriculum in the UK – something that would be valuable down under too.
Please don’t muddle along disturbed by your sudden outbursts of rage or misery-inducing depression. As you make your way through perimenopause and menopause, we believe your ability to function well in the world should be respected and you deserve to be well informed and that’s why we exist. To educate and empower you.
Disclaimer: Our articles are for information only and intended to educate from a holistic point of view. They should not take the place of medical advice. Certain diet and exercise practise may be beneficial for the majority of people but could have potential risks for others. If you are contemplating lifestyle changes or you have ongoing concerns please consult your healthcare provider.