Gut Feelings 💙
Q: I’ve got diarrhoea, could it be related to menopause?
A: Yes, it could be.
If you’re in pre-*, peri- or post-menopause and your gut’s playing up, you’re not alone.
In fact, digestive drama is suprisingly common during this phase of life. We’re talking acid reflux, bloating, constipation, diarrhoea and gas. Yep – the whole gut gang.
The good news? You can shift things in your favour by supporting three key areas:
👉 your gut microbiome
👉 your stomach acid levels
👉 possible food sensitivities
When you do that, amazing things can happen. We’ve seen women reduce symptoms, sleep better and even lose weight – true story! 😊

Why does digestion change during menopause?
It mostly comes down to the declining levels of estrogen and increases in cortisol that begin during perimenopause. Subtle signs can start early.
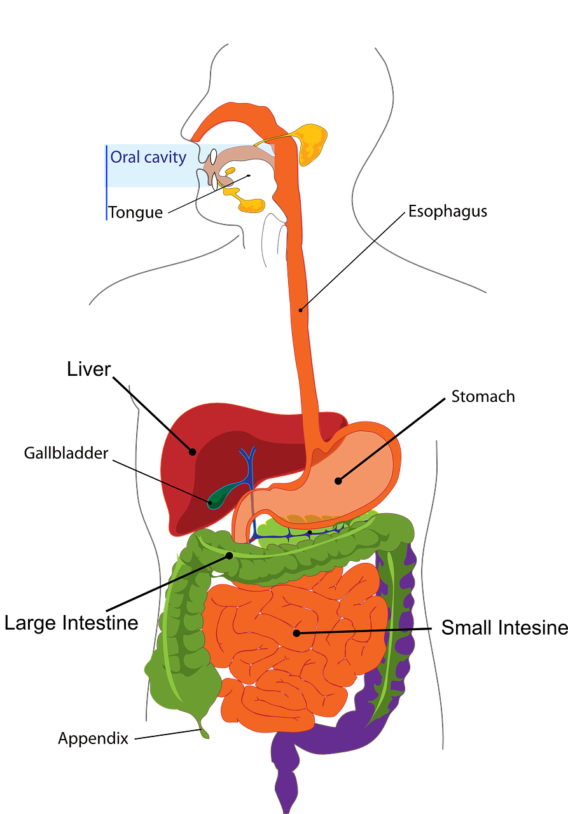
Your digestive system’s job?
Turning your meals into the nutrients your body needs to thrive.
It all starts in your mouth – chew, swallow, and voila – your food begins its journey through the gastrointestinal (GI) tract (that’s your gut, btw!). From the stomach to the intestines, it’s broken down and sorted so your body can soak up all the goodness.
And here’s where your gut-loving BFF comes in: dietary fibre. It keps things moving smoothly through your digestive system so your body can say “thanks, but no thanks” to what it doesn’t need – 💩 included!
The gut isn’t just a food processing machine – it’s also home to your gut microbiome (aka gut flora).
Inside your belly lives a bustling community of trillions of bacteria, fungi, and even viruses – more than the number of cells in your entire body. Some are the good guys, some not-so-much, but here’s the trick: they need to live in balance.
💙 When things go smoothly, they work together in hormony. But when they fall out of sync (like frenemies having a spat), it creates an imbalance. called gut dysbiosis. And that can lead to some not-so-fun issues like bloating, weight gain and IBS.

What happens to your gut during menopause?
Let’s break it down…
- As you ease into perimenopause, your entire digestive system starts to slow its roll. And that includes a drop in HCL (stomach acid) and digestive enzymes – the dynamic duo that makes up your gastric juices. These are crucial for breaking down food and keeping unwanted bacteria at bay.
- Another key player? Bile – made in the liver (see image above) and stored in your gallbladder, bile helps break down fats. As a result of menopause, it’s production often takes a dip. And that means your body might struggle to digest fats and fat-soluble vitamins like A, D, E and K.
- The result? You might suddenly find that foods you once loved (hello dairy, gluten, sugar and meat) don’t love you back. Your gut just can’t break things down like it used to – so nutrient absorption takes a hit.
- This matters, because your estrogen balance, adrenal function, and thyroid health rely on a steady supply of nutritional all-stars like: Zinc, magnesium, vitamin C&D,iron, calcium & selenium, folate and vitamins B6&B12.
Basically, poor nutrition leads to imbalances in gut flora. And if you add a diet heavy in processed foods and sugar into the mix you’ve got the perfect storm for weight gain, the symptoms we talked about above and hormonal imbalance. Indeed, when your gut’s under pressure, your whole system feels it – but with the right support, you can nourish your way back to balance.
Photo by Sarah Chai from Pexels

Let’s chat about stress, gut health and menopause

It’s a trio that’s more connected than you might think.
Here’s the scoop: stress is one of the biggest destroyers of healthy gut bacteria.
Yep, it’ s not just what you eat – your feelings play a major role in your gut health too.
Emotional and psychological stress can totally throw your digestive system off balance. And during menopause this impact is magnified.
When you’re stressed, your adrenal glands pump out cortisol – your body’s built-in alarm system. A little? Helpful. Too much? Not so much. And let’s be real…in today’s fast-paced world, we’re often dealing with way more than our fair share.
That’s why managing stress isn’t just good for your mood – it’s essential for your gut and hormones too.
One of estrogen’s many superhero roles? Helping to keep cortisol (your stress hormone) in check.
But during menopause, as estrogen levels drop, cortisol regulation gets a bit wobbly – which is one reason why stress can feel so much harder to handle in midlife. It’s not just you…it’s your hormones!
When cortisol kicks in it puts your body into fight-or-flight mode, flooding your bloodstream with glucose so you have the energy to run for your life – whether it’s from a tiger or a tense convo with your partner. (Cortisol doesn’t know the difference.)
The catch? When you’re in survival mode, digestion gets bumped off the priority list.
Over time, this can lead to digestive imbalances and sluggish gut motility, meaning food takes its sweet time moving through your system. Hellooo bloating, discomfort, and more…
Signs of a healthy gut
- No bloating
- No unwanted toots (aka gas-free vibes)
- No indigestion or heartburn
- Regular, easy-to-pass poops
- Soft/well-formed stools
- No visible, undigested food in the toilet bowl (sorry for the ick factor!)
What can you do to heal your gut?

- Avoid sugar, dairy and wheat
- Ensure you eat plenty of good fibre – fruit and veg skin, oats
- Drink lots of water
- Chew well – 30 times is optimum
- Try adding fermented foods such as sauerkraut or kimchi to your day (avoid this if you’re histamine intolerant)
- Don’t underexercise or overexercise
- Move your body with moderate exercises such as yoga, swimming or walking
- Avoid stressful situations as much as possible
- Incorporate more phytoestrogens, protein, fat and fibre (PPFF) in your diet. Read more about PPFF in 5 Ways Your Diet Should Change As You Enter Perimenopause
- Consider helping your digestive system with Happy Go Tummy®, our amazing prebiotic/probiotic combination. So it feeds the good bacteria (prebiotic) and increases them (probiotic). As such, it helps to ensure happy flora in the gut and the vagina. (Yep, the vagina has microbiome too!)
- In addition, Happy Go Tummy® helps you poop and increases your immunity. Indeed, these little babies (capsules) are powerhouses of goodness.
Conclusion
That so-called ‘gut instinct’? It’s not just a saying – your gut really does talk to you..
And learning to listen is especially important when you’re in pre-, peri- and post-menopause.
* We mention pre-menopause because giving your gut some TLC early on sets the stage for smoother transitions ahead.
But here’s the thing – gut symptoms can be tricky. They’re not always menopause-related. Medications like antibiotics, HRT, and the pill can play a part. So can how active you are (or aren’t).
And certain health conditions – like liver or bowel disease, diverticulitis, or even some cancers – can mimic menopausal digestive issues. Same goes for Crohn’s, coeliac disease, IBS and SIBO, These all need a proper diagnosis from your GP or gastro speicalist.
Bottom line: if your gut’s grumbling a little too often, or something feels off – don’t ignore it. Your body’s asking for attention. 💙
PS: Need a little gut love? Our digestive support bundle has you covered – tap the image below to take a peek.
Just so you know: this article is written by a real person who has studied the physiology of menopause and women’s healthy ageing. While we may use AI as an assistant, the research, insights and heart behind every piece comes from us.











