Webinar – Let’s Talk About Menopause
Replay
Did you miss the webinar? No problem.
You can watch it in your PJ’s.
Transcript
Hello and welcome to the Let’s Talk About Menopause masterclass, because it affects 100 % of the population.
Now it’s often mooted that it affects 50% of the population, which is true, and that it is women that experience it, but it also affects the men we love, the men in our lives, the men we work with, our friends, our family. So we kind of say that it affects 100 % of the population.
This is an overview of menopause, going through some of the signs and symptoms. A few lifestyle tweets you can do to help your journey go a wee bit smoother if you are someone that experiences symptoms. And please don’t hesitate to ask any questions or ask for any links or any information I’ve shared.
Can I just introduce myself to you and also MenoMe® so you can understand where we sit in this menopause space and where we’re coming from. So my name is Jenna Moore and I’m an accredited integrative health and menopause coach. I put on 20 kilograms and felt like I lost my mind when I stumbled into peri.
And I use the word stumbled intentionally because I had no idea to expect it even though I had worked in the women’s health and beauty industry for most of my career. I know that it’s true of a lot of my peers and certainly those that weren’t even exposed to that industry as well.
So something that can happen when we go into menopause is we become pro -inflammatory, in that we are more susceptible to systemic inflammation. We can also be susceptible to something called musculoskeletal disorder, which is pain in connective tissues, bones, joints, etc. And I believe also menopause has even been linked with fibromyalgia in some cases. And I experienced this very severely. So, severely in fact that I was pretty much immobilized. So what I did was I went back to the study books because I couldn’t find any answers and studied to be an integrative wellness coach which looks at the big picture not just nutritional awareness and movement but also spiritual things, community things, breath work, different modalities, a whole lot of different modalities and also working with behavioral science and habits, helping to form new habits.
I went on and studied women’s hormones through a functional medicine lens as well. And I actually haven’t stopped. I’m by no means a medical professional. I do come from a holistic integrative lifestyle medicine viewpoint, as does MenoMe®.
I work with MenoMe® and we are ‘by women for women’. We have women in their 30s, 40s, 50s and 60s on our team. And we’re pretty passionate about supporting women from pre -menopause right through to post -menopause with evidence -based natural solutions and also education. The education side of the business is very important to us because certainly from my own experience, but all of us have been through it or are going through it and are very open to learning about it. We believe when it comes to menopause, knowledge is power. And I will underline that with some of the stories I share with you.
Let’s just look at the basics first.
Menopause is the end of fertility. Not every woman will experience pregnancy during her lifetime, but if she lives long enough she will go through menopause. And it’s actually estimated that 1 .1 billion women will be in some form of menopause by the year 2025.
And when I first started talking about that date, it blew my mind because it seemed like years ago, years in the future, but in fact now it’s less than six months away. So that’s a whole lot of us.
There are four stages of menopause. Depending on who you talk to, some people abbreviate that, some people expand that. But we come from the pre -menopause side. Women are still having periods and no symptoms, although progesterone can drop around the mid 30s. So there can be subtle shifts, but not so much that you’d notice. Then we go into perimenopause. Again, you’ll hear different figures, but these are really good guidelines what I’m giving you here. So it (peri) lasts on an average to four years, but can last for over a decade because I certainly know it has for me. Now this can happen around 35 to 45. 35 being a very early part of that scale, early to mid 40s being more common. It can also taper off at the other end as well. I was listening to a beautiful holistic specialist, Dr. Holland of the Holland Clinic in Melbourne the other day, and she says she distinctly see’s three ages where women seem to come face to face with symptoms and that’s 35, 43 and 47 which I would concur with because I was 47 when a lot of what I just shared with you began happening to me.
Menopause itself is defined as 12 months with no bleeding or no periods.
In the Western world, this happens around the age of 51, 52, and other cultures that can be earlier or later. But by the time you know this, you are already in post-menopause. And then post-menopause is a time when most symptoms ease, a lot of women report feeling a lot happier. However, something to be aware of is that we become at increased risk of things like heart disease, hypertension, osteoporosis, which is a weakening of the bones, and more susceptibility to fractures, dementia and Alzheimer’s and type 2 diabetes. Now this can also fall under an umbrella term, which is known as metabolic syndrome.
With all of these averages here, we are just talking averages and we’re talking natural or spontaneous menopause, not early or premature menopause or surgically induced menopause because they’re a little bit of a different story. And I should point out that the SWAN study also identified early and late stages of both peri and post menopause and symptoms clusters. I’ve seen that myself, so I would agree as well.
To the changes, what’s happening? Progesterone is dropping, as I say, around mid -30s. This drops quite smoothly. A little bit later, estrogen begins to leave the building, and I’ll explain that in a moment, but it fluctuates, it can fluctuate quite wildly, it’s often likened to a roller coaster ride, so it can contribute a lot to the menopausal chaos or the symptomatic chaos that can occur at this time, which can be quite challenging for people. And it throws all the ratios out of kilter. Now, just a word there, there are two ways of spelling (o)estrogen, Eastern British spelling, which we tend to use down under uses an O in front of the E. Our style is just to use the E because we do go out all over the world but it’s the style that we’ve always used.
When we talk about estrogen it’s not always known that it’s a family, we have a family of estrogens. Estradiol is most dominant during our reproductive years and this is what is leaving the building, so to speak. And estradiol is beautiful, it’s very protective, it helps with a lot of our regulatory processes in the body and I call it our juice in that it helps keep our skin nice and plump and our joints and ligaments loose and flowing, it’s pretty important hormone to us. Then we have estriol, which is most common during pregnancy. Then estrone, which becomes our dominant estrogen during post-menopause. That’s a weaker form of estrogen, but we still do have some estrogen in our bodies.
This is a diagram of the stages we go through during the transition.
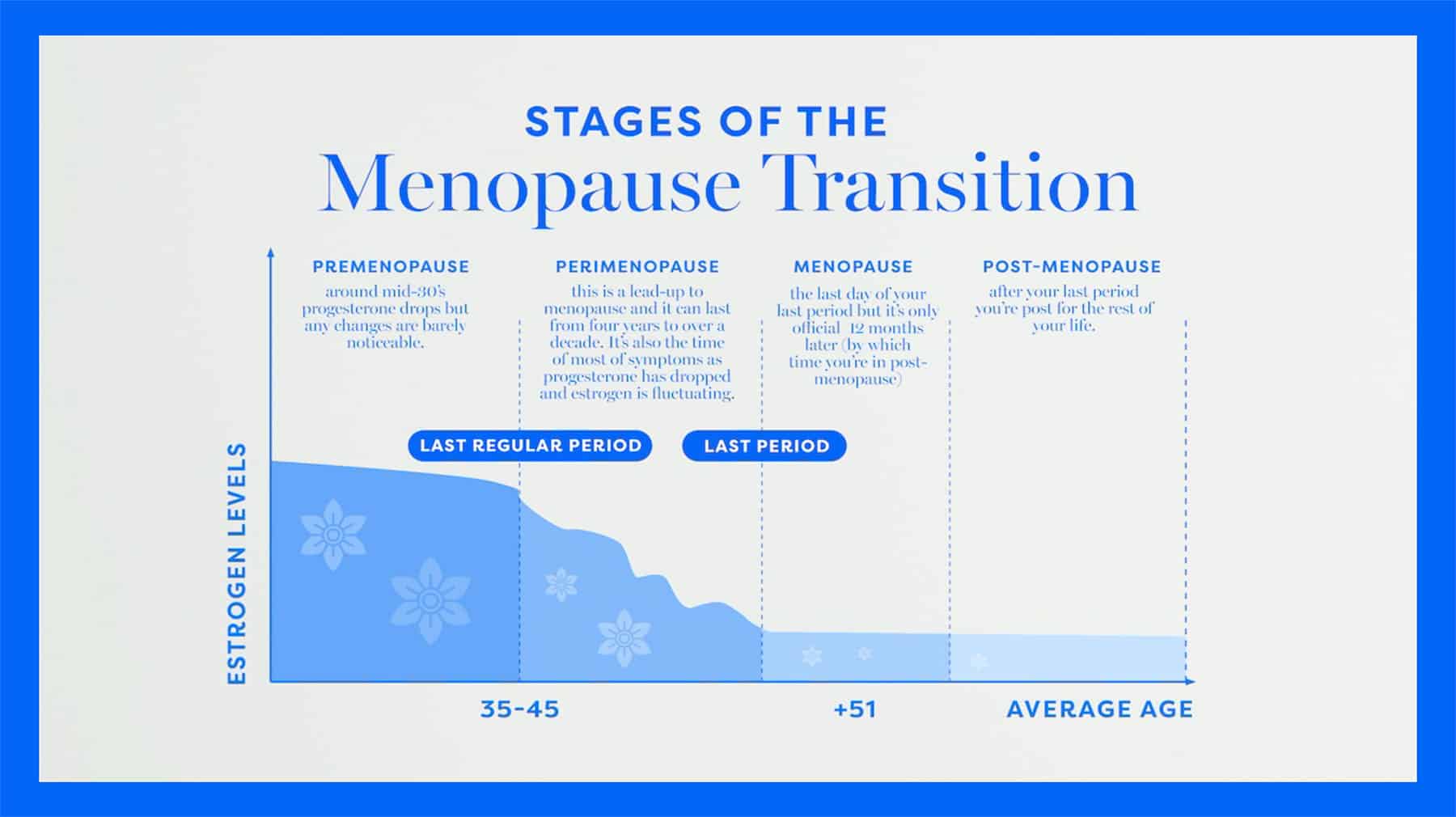
Pre-menopause, perimenopause, menopause and post-menopause. If that’s of interest to you, perhaps screenshot that because I think it’s quite a good reference point. It should be noted that there is no reliable test for peri, which makes it so hard because a lot of the symptoms can overlap with other things and it can be one of the reasons that we don’t know what’s going on. But because of those fluctuations, blood tests are not considered reliable by menopause societies.
Wonderful new research that was only published in June 2024 from Dr. Lisa Mascone, who’s a neuroscientist in the United States was measuring estrogen levels in the brain for the first time ever. She spent five years doing this and a lot of the data that came out of that was groundbreaking research. It’s set to change the face of menopause in the coming years. But one of the things that came out of that was that her measurements could 100% determine a woman’s menopausal status.
So there could be potential for a brain test, which is pretty exciting news for up and coming generations, because if we know what we’re dealing with, we’re a lot better off.
On the subject of blood tests though, they can be very useful for ruling out other things, because as I say, some of the symptoms can absolutely overlap with pregnancy, but also some autoimmune conditions and thyroid and gut issues. Blood tests are also very important for measuring your baselines that you need for health. But menopause societies suggest going by how you’re feeling and they acknowledge that you know your own body best.
The Australasian Menopause Society has a downloadable symptom checker on their website that you can use or you can take to your doctor. MenoMe® also has a quiz on the website that you may find helpful as well.
So what exactly is menopause?
Well, we’ve covered a lot of that, but it’s often referred to as second puberty because as we go into puberty, that’s a bit of a process as we go into our fertile years, the reduction in our reproductive hormones as we come to the end of fertility at the other end of the scale is what menopause is.
As I mentioned before, we hear a lot about estrogen, which is often meaning estradiol, but progesterone, which I touched on, is also a big part of this. Progesterone is beautiful, it helps us fall pregnant, stay pregnant. It’s often called nature’s valium because it helps us relax. And as that declines also, that can be behind very heavy periods, which we’ll talk about a little bit as well. Then testosterone is also key here and testosterone and androgens are known as male hormones but in actual fact we have three times more testosterone than estrogen pre & peri so it’s a pretty important female hormone as well and that helps with things like muscle tone motivation and libido.
HPAGT axis and the gut brain access come into play here. HPAGT stands for the hypothalamus and pituitary gland in the brain. The adrenals, because they are a big part of this, sit on top of our kidneys and they release cortisol, which is often known as our stress hormone. And it’s certainly our survival hormone, but we also need it. It gets us up in the morning and it motivates us. So it’s wonderful hormone.
GONADS, G stands for GONADS, which covers both testes and ovaries. Obviously in our case, we are referring to ovaries and thyroid because as I mentioned before, thyroid plays a big role here. In menopause, we naturally get increased levels of cortisol, so we tolerate stress less and the thyroid is very sensitive to stress. It also loves progesterone.
As our progesterones declining, for many women going into perimenopause or midlife, they can develop underactive thyroid or hypoactive thyroid, hyperactive thyroid as well, but hypoactive tends to be the more common one. So that’s something to be aware of as well. It’s a gradual, multilayered, rather complex biological process.
It’s not an overnight thing which I think some of us know, I certainly did, I thought it would happen way off in the future when I was old. But perimenopause can be challenging, confusing and overwhelming for many women and it’s quite famous for that now, but not for everyone. In fact, 20% of women sail through, they don’t experience any symptoms and they wonder what all the rah rah is about.
However, 60% of women experience moderate symptoms and 20% severe. In fact, I heard a well-known American influencer yesterday call it brutal. And it can be, I would agree with that. But that’s 80% of women that experience some sort of disruption in their life. And it’s certainly not brutal for everyone, but for some of us it is.
So it is something to look at, it is something to talk about. The wonderful thing is that we are talking about it now and when there’s more conversation out there, there’s more solutions and there’s more support.
Menopause itself is only a moment in time, which I referred to before, the last day of your last period. But a US study found that 45% of women don’t know what perimenopause is, just like I didn’t. And like I say, that’s hard to believe when you think of the industry I’ve been in, and I’ve done a lot of breast cancer work too, which can be related in terms of women’s biology and physiology and the hormonal aspects of that.
It wasn’t very long ago that I was helping a woman and she was telling me what she was experiencing and I said to her, that sounds like perimenopause and she said, excuse my ignorance, but what is that? So it is still very much an unknown in some circles. Hopefully we will be breaking through that unawareness because once we create awareness of something, we can break the cycle. And we did do that with breast cancer actually.
So that same (US) study showed that 73% of women are choosing to tough it out. And I find that very sad because 80% of women are experiencing some disruption in their life. And there is so much out there now, whether you want to choose medicine, if you want to use natural alternatives, if you want to use what’s known as woo woo, if you want support groups, it’s all there for you.
I hope Dr Linda Dear, also known as the Meno Doctor, the lovely Dr Linda Dear doesn’t mind if I use her analogy and she talks about a menopause buffet. So we’ve got this buffet in front of us and we can go there and pick and choose and see something that lights us up or we feel might work for us and give that a go. If it doesn’t work for us or we don’t like it, we can go back to the buffet and choose something else and I think that’s a wonderful analogy. So thanks Linda.
So a little bit of a word about HRT or MHT. HRT stands for hormone replacement therapy. Menopause hormone therapy (MHT) is the more modern term but it doesn’t seem to be gaining much foothold right now. I’m certainly not a medical professional, but I know that there’s so much talk about it out there. It’s probably a question you’re going to ask. So to be clear, that’s not our scope of practice. It’s not something we’re qualified to talk about. But it isn’t a magic pill, it seems to be talked about as if it’s a panacea, but it’s not a magic pill. That said, it is helping so many people, which is really wonderful. It may not address every single symptom though, and things like hair thinning or gut issues may require other support.
And also Professor J .R. Shrikulkarni, who’s a wonderful woman at Monash University and Melbourne says that whatever solution you use, really needs to be able to cross that brain barrier as well. I’ll tell you a little bit about her more in a minute. So it (HRT) is great for many women, but it’s not for everyone because some women can’t take it and some women do not want to take it. And we hear that from women they don’t do well on it, which is what Professor Kulkarni has said in terms of mood because she specialises in the link between women’s hormones and mental health. So it’s really a conversation to have with your medical professional who is certainly far more qualified to talk about that than I am.
There are 34 recognised symptoms of menopause and counting and I say and counting because this is from when I started a decade ago in the space and menopause was still very much swept under the carpet, wasn’t being talked about like it is today. And this was the general consensus. This has changed, this has changed even in my own data and work and information gathering. And I’ve got a list of the 34 coming up for you, but I’ve got add-ons to that. And you will often hear 66 as well and there’s a company in the US that have counted 101 symptoms. So things are changing, we are learning more and it’s not just about hot flushes. So this is a key message. Menopause is not just about hot flushes and most of these things occur, most of these signs and symptoms occur in perimenopause, not all.
But most often some of them will settle down again in post-menopause. Again, not all, but some. A lot of it is due to that hormonal chaos and fluctuations and roller coaster I mentioned before. None of this information is to scaremonger as we go through the symptoms, it’s more that knowledge is power. I will share some stories of women as we go through the symptoms. So that really underlines it because where you may experience what they did, hopefully now you’ll know that it could and nothing is a hundred percent in health, but it could link in with menopause rather than something more sinister.
We have estrogen receptors all over our bodies, including our brain and our gut and so a lot of the signs and symptoms are both physical and psychological because our central nervous system is affected here as well. And in the past, a lot of people might have just thought it was related to physical symptoms or maybe mood swings in there as well. But mental health is a very big part of this, which is when I referred to Professor Jayashree Kulkarni before, is something she specialises in. She’s created groundbreaking research for the worldwide specialists on this and I host a podcast called Women on Fire® that MenoMe® sponsors and she was a guest on there a few episodes ago. So if this is something you have an interest in I would really encourage you to go and listen to that.
So part of these psychological symptoms are anxiety. Now this is a very common one. I had a friend that experienced this and she couldn’t
drive for four months and she was in and out of hospital thinking she was having heart attacks. This is the same for panic attacks. A lot of
women feel like they are having a heart attack or something more sinister is coming on.
And it’s important to recognize that depression can come back during menopause, especially if you have experienced it before. So that’s
something to take notice of, and also ACEs, which are known as adverse childhood experiences. If you’ve had any of these and you haven’t dealt with them, they can show their head at this time science is showing.
Now, Professor Kukani says that menopausal depression, is also sometimes called menopausal mood disorder, is very different from standard
clinical depression. So it’s important to recognize that as well. And the other thing with the signs and symptoms, it’s not just about sex hormones. So it’s to do with the brain and the gut, the cortisol that I mentioned before, insulin, which is blood sugar, and thyroid.
So that’s why there is a vast array of symptoms and we are finding out more and more. Now the thyroid, it’s worth mentioning that the
thyroid also governs metabolism and weight gain is common at this time and I do know it’s one of the biggest bug bears for women. It’s
something I specialize in. It can be managed definitely, but it is in terms of understanding it and it’s a whole master class on its own.
So if you want to know more about that, don’t hesitate to get in touch.
So let’s go through some of these common symptoms.
Aches and pains, particularly in the joints and muscles. You might’ve heard me mention musculoskeletal disorder right at the beginning when I was talking about my story. So it’s very common to get these in the fascia, which is your tissue between your epidermis or your outer layer of skin and the bone. That’s what I experienced. A lot of women feel like they’ve overdone it in the gym when in fact it is linked to shifting hormones.
Allergies, you may not have experienced an allergy before and all of a sudden experience them now. That’s not uncommon.
Anxiety, we have mentioned.
Bloating, can be linked to gut issues. It can be due to other things as well. Also, we can become more sensitive to some foods, particularly things like gluten and dairy. So that’s something to monitor to see how you’re faring when you are eating those foods.
Body odor changes, which surprises a lot of people.
Brain fog. This is quite a common one, and a lot of women fear that they are getting early onset dementia. And quite often that’s not the case. And as I say, Dr. Lisa Mascone’s research really did show that a lot of symptoms do begin in the brain and it’s also why Professor Kulkarni has said it’s important for whatever aids you use that they can cross that brain barrier.
Burning mouth syndrome, which can feel like burning mouth or a metallic taste in your mouth.
Depression, which I’ve talked about.
Digestive changes, which I’ve talked about.
Dizziness also very common. We have a big library of blogs on the website. Dizziness would be one of the most read. So it’s very common.
Electric shock sensations, which can feel like electric shocks against your skin.
Facial hair, which can be due to do with that androgen testosterone male hormone ratios.
Fatigue and tiredness. This can be a biggie. And I did hear recently that chronic fatigue is now being linked in some cases.
Feelings of dread and doom.
Formication, is a sensation of crawling bugs under the skin.
The infamous hot flushes.
Hair thinning and hair loss. Now this can be due to stress or nutrient deficiencies as well, but it can also be hormonal.
Headaches and migraines, can become common. The good news there is they should settle down in post-menopause.
Heart palpitations or panic attacks, which I mentioned before are very concerning for some women who find themselves ending up in the A&E.
Incontinence, urinary incontinence. So if you have given birth, you may have experienced stress, urinary incontinence when you cough or sneeze or you have a little leak. Whoopi Goldberg calls it peezing. Urgent continence is a little different. You might be putting your keys in your front door, you might be about to drive your car, you might be in a queue to purchase something at a store and all of a sudden with no warning you have to go and you have to go right there and then. So that’s very discomforting if that’s something that you experience.
Insomnia and sleep issues are very common.
Really the first signs of perimenopause are irregular periods or change in flow. As I said, developing very heavy periods or flooding can be very concerning for some women and that has been linked with the lower progesterone. So that can be a bit of a concern. A friend of mine was flying to the UK and wearing white jeans and this happened to her. So it can be very distressing depending where you are.
So irritability is another one and we can get a very short fuse. I’ve heard of many women who say that all of a sudden they cannot stand watching or hearing their partner chew, whereas for years before it’s never bothered them.
Itchy skin, and this includes the vagina as well. This is a very common one too and it’s quite crazy making, think I’ve certainly experienced it. And some women can scratch themselves raw. Vitamin C can actually help with this and there are some other helpers as well. We do have a blog about that on the website.
Loss of libido is common and a concern for a lot of women or a lot of their partners. But the other side of the equation is not as common, but some people get increased libido as well.
And mood swings where you can experience tears, joy and rage in the space of a few seconds which you might have experienced in pregnancy or with PMS as well. Rage very much consumes a lot of women because it can affect their relationships and affect their family life. So that’s something to be aware of. You just want to find ways to chill. That’s why me time and self care becomes very important.
Muscle tension because your muscles are changing at this time.
Night sweats, which can be soaked linen, I feel fortunate that I’ve never experienced that.
Oral changes which can include bleeding gums and broken teeth, so it’s very important to keep up your regular dental appointments.
Sore breasts which can be linked with a lot of estrogen, high estrogen on the ratios. This is often called estrogen dominance, some people don’t like that term. I think it’s kind of fitting.
Tingling extremities or numb hands and feet this is known as peristhesia.
Trouble staying asleep and I’m going to talk about the circadian rhythm so I’ll give you a little tip there but a lot of women find that they wake up between about two and four.
Recurrent UTIs or urinary tract infections and vaginal dryness. Now the pH levels are altering in the vagina which can contribute to this and so that’s 34.
But wait there’s more!
Like I said to you before I just had to add some more. So tinnitus which is ringing in the ears that can definitely be linked to menopause and a lot of people don’t realize that.
Weakened fingernails, weight gain which we’ve talked about. Burning feet, introversion, very common where you may not want to attend social engagements or see friends and I should put a slash there and put loss of confidence because loss of confidence is very key as well, very common as well and that can be a big hindrance to careers.
Osteoporosis which we talked about, smelly pee so pee can take on an ammonia like smell, overactive bladder and suicide ideation which links into Professor Korkani’s work. And in Australia, the most common age, because we have the data, but this is probably true for New Zealand and the world as well, and we have seen that in some high profile women of this age, but the highest age group to take their own lives is women aged 45 to 54. So that’s right in this perimenopause bracket.
So that’s something to be aware of and why mental health is so important to underline at this time.
Vaginal atrophy and prolapse, which can feel like your vagina is falling out. And I know that does not sound good. The wonderful thing is there are a lot of specialists out there now who can help with some of these things. And also there are lifestyle practices that can be an aid as well.
But that’s where lifestyle medicine comes in because it’s really important to note that a lot of these symptoms can be magnified by things like poor diet, nutritional deficiencies, sleep issues and chronic stress, toxins from the environment, plastics and personal care, which I’ll expand on in a little bit, the wrong type intensity and duration of exercise, poor liver, adrenal and thyroid function.
Gut issues, which links back to nutritional deficiencies, because if you do have gut issues, you may not be absorbing your nutrients as well, and insulin resistance, which is blood sugar issues. We naturally become more insulin resistant at menopause.
So genes load the gut and lifestyle pulls the trigger.
It’s which do suggest talking to your mama if she’s still alive and asking her what her journey was like. Don’t you love the energy of the slide though? It’s so beautiful. But lifestyle pulls the trigger. The choices we make in our lifestyle can either magnify or mitigate some of the signs and symptoms, which is very interesting, isn’t it? Many women are affected by these symptoms, as I mentioned before, 80%.
and some leave their relationships and I did that. Careers, especially due to that lack of confidence or loss of confidence or consider suicide. So they are very real for women who are experiencing them. The wonderful thing is that mainly we do come out the other side. But yeah, always reach out and support other women if you can.
If you want to tweak your lifestyle, if you want to try and improve your journey, take a look at things like how you manage stress and also sleep, because those two are very interlinked. Sleep is very crucial during this time because that’s our regenerative time. And if we go without sleep, it’s very difficult to function the next day, but sleep disruption is very common at this time.
Also, as I mentioned before, we get the higher cortisol. We are meant to be in survival mode sometimes, but not all the time. So if we can bring in some rituals or practices that help reduce this, and there are a few and I’ll share a couple with you in a moment, that’s a great thing. Then take a look at your food and lifestyle. As I said, you know, some of our lifestyle practices and food actually plays a big role can really affect our symptoms. Triggers for things like mood and hot flashes and so much more can be refined in added sugars, alcohol and caffeine. These also load down the liver and the liver is a very hard -working organ and one of its jobs is to metabolize and help excrete estrogens that we don’t want.
And if it’s loaded down, that can’t do that. Other things that load down the liver, toxins that I said I would expand on. Now these are called EDCs and endocrine disrupting chemicals and Xenoestrogens. You will find them in personal care, your makeup and your skincare and your hair products and your cleaning products and in the environment. If you can choose as natural as you can, the better off you are. Some of the chemicals in these products are ADCs and Xenoestrogens and they can mimic our natural estrogen. If the liver’s not doing its job, if it’s loaded down by these type of toxins or the sugars, the alcohol, the caffeine, then these estrogens will get reabsorbed and recirculated, and they’re all not only magnify symptoms, but it is being looked at by scientists as being a link between some conditions such as cancers. So that is something to be aware of.
As a health coach, we always suggest baby steps for changing habits and not changing everything overnight because that’s just too hard for humans. It’s too overwhelming. But if we can implement a few little steps at a time, we have far more success. So some of these things you may be doing, some them you may not. So just choose a couple and try them out and see how you go. They’re certainly not mandatory to anyone. That’s all personal choice. So eat more good stuff.
We focus on the Mediterranean style diet, which is unprocessed whole foods, lovely lean proteins, healthy fats, low glycemic carbs and fibre. Most of the world’s population don’t get enough fibre these days, which is linked with a whole lot of malaries and we have more and more autoimmune diseases emerging all the time.
Now the Mediterranean style diet looks at things like seven to 10 series of fruit and vegetables a day that’s super rich in fibre and lots of beautiful high high quality extra virgin olive oil and things like avocados, berries and low glycemic carbs like say oats are really good there. It’s quite famous for having some alcohol in there isn’t it but it’s usually just one glass of wine and it’s usually ingested with food, which helps it all be processed beautifully.
Hydrate, natural filtered water, pure filtered water is your best bet. Natural moisturising factors reduce as we age, and hydration is very key to our wellbeing. I think we all have heard how we wouldn’t survive very long without water. A beautiful way to start your day is with some sliced lemon or grated ginger in lukewarm water. Your digestive system loves this. Also, your liver loves this and it helps with your hydration. Hydration helps with energy. It helps with bowel movements, and certainly bowel movements are very, very common in menopause, be that diarrhea or constipation, more commonly constipation. So it helps with that, helps with skin. It just helps with so much. Hydration is one of the basics of life.
Move moderately and first thing is great. It’s wonderful that there are some specialist exercise trainers out there now, so if that’s something that you want to look into it’s probably a very good idea. But moving in the morning at first light without sunglasses for about 15 minutes is fantastic as well because it links in with our circadian rhythm which I’ve got there at number four if we can work with that. So our melatonin hormone starts being released and produced around 9pm at night. If we go to bed earlier around that time round 9 .30pm to 10 and go through the night and cortisol helps us get up and motivates us to get out there at daylight. But what you’re doing by getting out there at first light and without the sunglasses is you’re helping increase the levels of the hormone adenosine which is the one that helps us stay asleep through the night.
Also loving your liver, which I talked about before and that’s certainly a whole other subject on its own as well, will help you sleep through the night as well. And then if you needed some instant first aid with anxiety or a panic attack, there are a couple of breathing exercises you can do. Longer form breath work is wonderful for you as well and yoga has some wonderful breath work, but a couple of very short first aid ones are breathing in for four, holding for seven, breathing out for eight, all slowly, and rinsing and repeating. Or there’s also the box breathing which is breathing in for four, exhaling for four, breathing in for four, exhaling for four, and doing this slowly rinsing and repeating.
And what these can do is work with the vagus nerve and bring you back into a parasympathetic state, which is your rested and relaxed state, and it works as pretty much magic, it works pretty instantaneously.
And then connection is so important, particularly if you’re experiencing that loss of confidence or that introversion, is to really connect with your girlfriends and people that you love, release the hormone oxytocin, which is known as the love hormone and the feel-good hormone really. So connection and community are key. Science has showed that isolation and loneliness can be a real problem for menopause on their own.
And then number seven is vitamin H which is vitamin humour which I love. We know in our community our ladies just love humour and science does show that women thrive on it and it gets them through challenging times in life, particularly if they’re having a challenging menopause.
So I hope that’s of help to you. As we come to the end, I wanted to share a gift that we have for you in celebration of Women’s Health Week. And so… we have 25% off all products excluding bundles with the code WHW25 (code expires midnight Sunday 18th 2024).
Now we have four, a little stable of four, LotsaLocks® which is amazing and that helps with hair thinning and hair loss if that’s coming from a hormonal perspective. Merry Peri® to support women during perimenopause. Perky Post® to support women during post-menopause and Happy Go Tummy® to support gut issues. Some of the ingredients here are amazing. I’ve been immersed in the data and we bring in a bit of that vitamin H into the products titles. So if this is something that interests you, please do take advantage of that beautiful 25% off and we would love to hear your feedback.
Thank you so much for joining me today. I hope you have gained some knowledge and if you have any questions or need any links to anything that I’ve shared, please don’t hesitate to reach out.
Mark your calendars, ladies!
Join Jenna’s special webinar during Women’s Health Week.
She’ll be covering all things menopause: what it is, the stages, eye-opening statistics, and lifestyle supporters that can make a big difference.
Tune in on Thursday the 15th of August at 12:30pm (NZT)
(Can’t attend live? No problem! Register and we will send you the replay straight to your inbox).