Lots and lots of women experience changes with menopause and gut health starting with perimenopause.
As a result, bloating, food sensitivities/intolerances, constipation, diarrhoea or reflux/heartburn (GERD) can raise their heads.
And oftentimes you don’t link your gut health with perimenopause, menopause or post-menopause.
I mean, why would you?
Unsurprisingly, you probably think of menopause and digestion (oh, and pooping!) as completely separate entities.
But they’re not.
Related: Out Darn Constipation, Out I Say!
Menopause and gut health: the estrogen effect
In fact, a healthy gut nicely populated with a diverse group of microbes (fungi, bacteria and viruses) is vital in every stage of menopause. (And life!)
This is because the gut microbiome is one of the main regulators of circulating estrogen. And certain bacteria and specific enzymes such as beta-glucuronidase convert estrogen into an active form1.
However, menopause is linked with less of these bacteria and by default less estrogen in the body. Are you with me so far?
Did you know? We have 1000 trillion microbes in the body.
Menopause and gut health: the brain connection
For this reason, the changing estrogen levels of menopause are affected by gut health. Cortisol (the stress hormone) also plays a role as when the body perceives danger it will always prioritise survival over digestion.
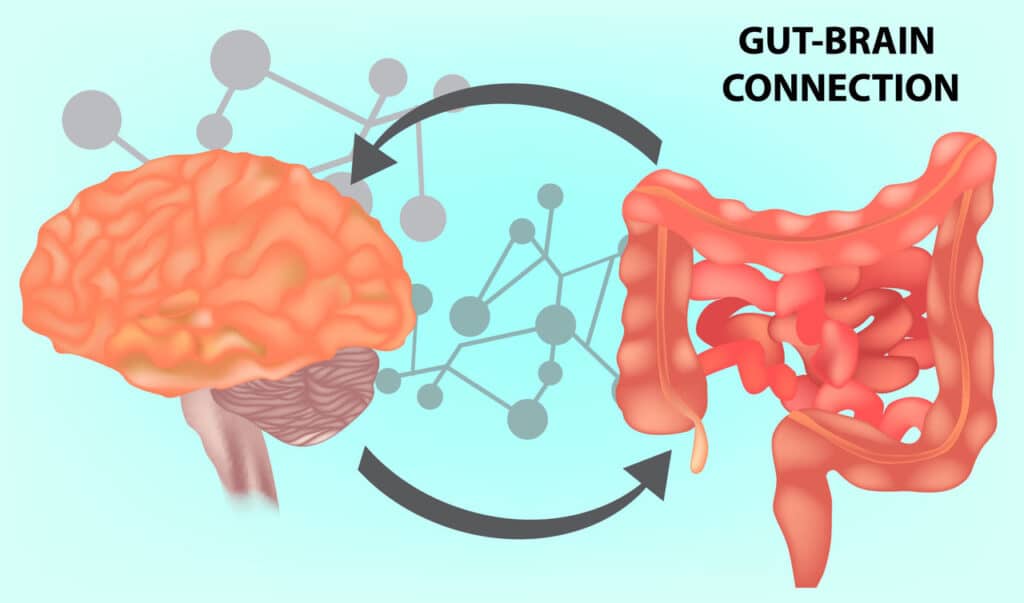
Furthermore, the gut has earned the nickname ‘second brain’ or – in science speak – ENS (enteric nervous system). And a gut/brain connection is now well recognised.
In fact, it’s known as the gut-brain axis.
So your digestive system, brain and hormones are all connected.
Although in scientific terms, this discovery is relatively new. Therefore, it’s transformed the way scientists understand the link between digestion, mood, overall health and well…yes…menopause.
Not least because microbiome dedicated to regulating your estrogen have been discovered. These microbiome – or family of microbes – are known as the estrobolome.
Menopause and gut health: meet the estrobolome
To clarify, the estrobolome is a group of bacteria dedicated to helping your body metabolise and regulate estrogen.
How incredible is that?
And bacteria in the gut and estrobolome can affect estrogen levels and weight, mood and libido.
So if you have a healthy gut during any stage of menopause it’s a sign the estrobolome is performing well. And it’s producing enough of an enzyme known as beta-glucuronidase. Indeed, it’s a bit of a mouthful, sorry!
Part of the estrobolome’s role is to support estrogen in circulating through the body. In addition, it helps take it to the liver to be processed before being delivered to the intestines where it’s excreted through poop or urine. Or, if this doesn’t happen, it’s recirculated which isn’t ideal.
A healthy estrobolome produces enough beta-glucuronidase to reduce the chance of reabsorption and help elimination through poop or urine.
But if there’s an imbalance in the gut bacteria – known as dysbiosis – beta-glucuronidase that isn’t performing well may cause estrogen to be absorbed back into the body.
This can lead to magnified menopausal signs and symptoms, estrogen dominance and – perhaps – the risk of disease.
An area of interest
For this reason, the estrobolome is an area of interest in hormone-sensitive cancers2, obesity, endometriosis3 and cardiovascular health. However, it requires much more study.
Did you know? 90% of digestion occurs in the small intestine.
Signs of dysbiosis
It’s tricky because some signs of an unhealthy gut can crossover with commonly assumed perimenopause/menopause symptoms. Including:
- Autoimmune conditions
- Bloating
- Constipation
- Diarrhoea
- Fatigue
- Food intolerances
- Gas
- Heartburn
- Weight gain
What causes an unhealthy gut?
- A low fibre diet
- Eating high sugar and processed foods
- Lack of healthy fats
- Minimal fresh fruit and vegetables
- Chronic stress
- Antibiotics and prescription medications
- Disrupted sleep
- Not moving your body regularly
Menopause and gut health: how can you improve your digestion?
While poor gut health can trigger (peri)menopausal symptoms here’s the good news – there’s a lot you can do!
The truth is, our modern lifestyles have taken away basic gut-loving tools such as fibre rich diets and swapped them for highly processed foods.
Additionally, our lifestyles are often filled with things that aren’t gut friendly such as stress.
But you can turn it around.
Studies have shown it doesn’t take long to get your gut back to optimum health after making a few diet and lifestyle tweaks.
And that means lower stress, happier moods and a more comfortable physicality. So why wouldn’t you tweak?
You’re not alone: Join Shake It Off® 10-Day Hormone Reset
Tweak your diet

Did you know? Gut bacteria love fibre and most of us don’t enough of it.
- Embracing fibre, phytonutrients and phytoestrogens as per our PPFF guidelines is a great first step. And if you don’t know, this means phytoestrogens, protein, fat and fibre.
Read: How Food Can Help You Have Your Best Menopause | Meet PPFF
- Green leafy vegetables as well as the cruciferous family such as broccoli, cabbage, bok choy, brussels sprouts and cauliflower are packed with fibre. (Lightly steam them for thyroid health.) Bitters are great too (the liver loves them) like rocket and dandelion.
- Phytoestrogens such as lentils, chickpeas, tofu, tempeh, flaxseeds and leafy greens are similar to our body’s estrogens. Although they’re much weaker they can contribute to a healthy estrobolome. According to Dr Aviva Romm, author of Hormone Intelligence, they can help us absorb and excrete the right balance of estrogen. “And here’s a win-win”, she says:
“Healthy estrogen levels in turn support healthy gut function. Estrogen helps maintain the health and integrity of your gut lining preventing a leaky gut.”
- Consider adding foods such as (prebiotic) garlic, onion, leeks, asparagus and (probiotic) fermented foods such as kombucha, kimchi and sauerkraut to your meals. Gut bacteria and the estrobolome thrive on prebiotics and probiotics encourage more good bacteria growth.
- This is why we created Happy Go Tummy™ our combination prebiotic and probiotic in a capsule! Click here to learn more.
- Lemon water or ACV (apple cider vinegar) are often touted as digestively beneficial and they can have mild benefits. However, they may not alleviate significant issues and could even aggravate GERD. So always ensure you dilute them.
- Herbal teas such as peppermint and ginger are good gut choices.
Try: Ginger Water
Things to avoid
1. White processed foods
The ‘whites’ such as white sugar, white pasta, and white bread can all contribute to the proliferation of unwanted gut bacteria. (The bad guys!) In addition, processed foods can reduce microbiome diversity and add to weight issues, systemic inflammation and leaky gut.
2. Nix alcohol
While many of us love our nightly vino it can magnify symptoms like hot flushes and sleep disruption. (Sorry!)
It can also increase gut permeability and inflammation, play havoc with our gut microbiome, the estrobolome and the liver. Therefore, the liver’s ability to detoxify estrogens including xenoestrogens and EDCs are impacted.
What’s more, it can raise overall estrogen levels which can increase (peri)menopausal symptoms and has been linked with hormone-sensitive cancers.
Read: Menopause & Alcohol – Is A Wee Tipple Helpful Or Harmful?
3. Watch out for environmental influences
Our world is awash with chemicals and substances that produce xenoestrogens or endocrine-disrupting chemicals (EDCs).
These are sometimes called ‘dirty’ estrogens, mimic our natural estrogen and are stored in the liver and fat cells. Therefore, they can disrupt the estrobolome as well as exacerbating menopause symptoms.
You’ll find xenoestrogens in cleaning products, personal care, fragrance, plastics and pesticides.
4. Be sparing with antibiotic use
There are times when we need antibiotics to help knock illness on the head. However, their use disrupts the gut microbiome and can contribute to dysbiosis4.
So it’s a good idea to add in the foods we’ve talked about under ‘tweak your diet’. Also, add in extra support such as a very good pre- and probiotic such as Happy Go Tummy™.
Interestingly, a study by the University of Copenhagen5 found that gut bacteria can recover after antibiotic use in healthy people. But after six months, the gut still missed nine common beneficial bacterial species.
Purchase Happy Go Tummy™ here.
5. Move your body
When we reach perimenopause and right on through into post-menopause our bodies thrive on regular, moderate movement.
And exercise supports liver detoxification and the work of the estrobolome.
Not only can regular exercise mitigate stress (and lower cortisol levels), it can also nurture your hormonal health. Especially exercise such as yoga, walking and Pilates.
Conclusion
So there’s certainly a direct link between menopause and gut health and peri/menopause symptoms, the estrobolome and overall microbiome.
The good news is it can all be improved via diet, lifestyle, movement and managing your stress levels.
So if you feel your gut health needs improving why not give some of our suggestions a go?
In addition, we have Happy Go Tummy™ to support your happy gut bugs.
Here’s to good guts!
Share with a friend
Sign up to our mailing list for the latest news and stories and receive a $5 discount code to redeem on your first purchase, plus receive a 3-step eBook on ways to support your body through menopause.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Related Articles
Sources:
Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017 Sep;103:45-53. doi: 10.1016/j.maturitas.2017.06.025. Epub 2017 Jun 23. PMID: 28778332.
Ervin SM, Li H, Lim L, Roberts LR, Liang X, Mani S, Redinbo MR. Gut microbial β-glucuronidases reactivate estrogens as components of the estrobolome that reactivate estrogens. J Biol Chem. 2019 Dec 6;294(49):18586-18599. doi: 10.1074/jbc.RA119.010950. Epub 2019 Oct 21. PMID: 31636122; PMCID: PMC6901331.
Le N, Cregger M, Brown V, Loret de Mola J, Bremer P, Nguyen L, Groesch K, Wilson T, Diaz-Sylvester P, Braundmeier-Fleming A. Association of microbial dynamics with urinary estrogens and estrogen metabolites in patients with endometriosis. PLoS One. 2021 Dec 16;16(12):e0261362. doi: 10.1371/journal.pone.0261362. PMID: 34914785; PMCID: PMC8675749.
Lange K, Buerger M, Stallmach A, Bruns T. Effects of Antibiotics on Gut Microbiota. Dig Dis. 2016;34(3):260-8. doi: 10.1159/000443360. Epub 2016 Mar 30. PMID: 27028893.
The composition of gut bacteria almost recovers after antibiotics. https://www.sciencedaily.com/releases/2018/10/181023110545.htm#:~:text=Summary%3A,nine%20common%20beneficial%20bacterial%20species.











